In an era of rising staffing shortages, patient safety is at risk. Workforce shortages, especially in the areas of nursing and nursing support, lead to potential risks including unsafe patient care conditions, delay of vital procedures, and staff unfamiliarity with high-risk processes.
Operational risks can include recalls and/or vulnerability alerts associated with medical supplies and equipment that may not be adequately addressed as well as the inability to monitor supply shortages that can lead to procedural delays and/or cancellations. Financial risks also exist, including costs associated with temporary staffing, procedural delays, and malpractice settlements.
This is why ECRI and the Institute for Safe Medication Practices (ISMP), the largest patient safety organization (PSO) in the country with a database of over five million patient safety events, named staffing shortages its number one safety concern in 2022.
Although healthcare staffing shortages have been pervasive for years, they have become amplified by the COVID-19 pandemic. Nearly one in five healthcare workers have quit their jobs since the start of the pandemic. Furthermore, registered nurses (RNs) are no longer delaying retirement, and it is predicted that one million nurses will retire from the workforce by 2030—taking their knowledge and expertise with them.
Not only are there staffing shortages in various healthcare roles, but there is also a shortage of expertise in those roles found across the care continuum. To further complicate the issue, organizations do not have applicants in the pipeline to fill these vacancies. It takes three months to recruit an experienced RN, contributing to a high RN vacancy rate. A lack of sufficient nursing school faculty has compounded the healthcare shortage by limiting growth of US-based nurse training programs. In 2018, nursing schools rejected over 75,000 qualified applicants.
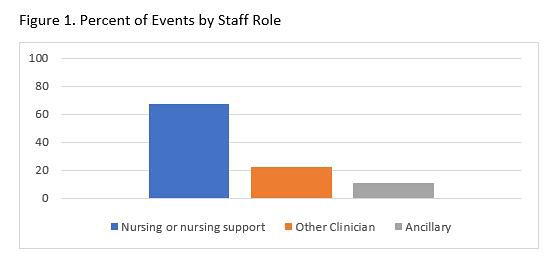
An in-depth review of patient safety events related to workforce shortages revealed that staffing shortages were most commonly noted in the role of nursing and nursing support, followed by other clinical and ancillary staff as shown in Figure 1.
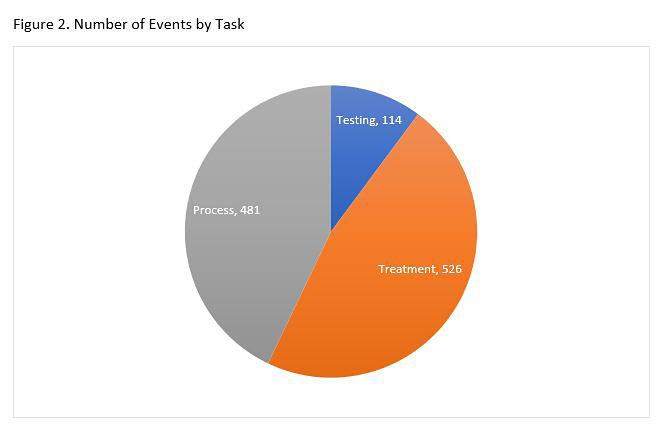
Events related to staffing shortages were grouped into three categories: treatments, processes, and testing. The majority of failure modes occurred in the treatment category, followed by processes, and then testing, as shown in Figure 2.
A Different Approach to Safety: A Total Systems Approach
The example of staffing shortages illustrates the system complexity that healthcare organizations and clinicians face today. Improving safety has been a national priority for more than two decades, since the report To Err is Human: Building a Safer Health System was published, shining a spotlight on the safety risks and harm that patients experience in the US healthcare system. Despite years of varied approaches including research, education, and public reporting, the risk of harm still exists. A recent study published by Bates and colleagues showed that adverse events were identified in nearly one in four hospital admissions, and of those events, almost a quarter were preventable.
As healthcare organizations continue to struggle to address safety concerns in a systematic way, siloed and fragmented efforts will continue to fail, and as we have seen with the staffing shortage crisis, there is no room for wasted time or resources. There is simply not enough time, people, or finances to support ineffective systems. A total systems approach to safety is driven by principles of system design, human factors, health equity, and advanced safety science. It takes into consideration different system factors—including the environment, people, tasks, tools, and human-machine interactions—that make up the care delivery process. Effective design operationalizes the integration of system factors to facilitate the way people, processes, equipment, technology, and leaders all work together to achieve better care in a safer environment.
Adoption of human factors engineering is becoming increasingly critical as the digitization of healthcare grows. Like other high-risk industries, healthcare has become increasingly dependent on technology. Understanding how humans interact with technology is essential for the safe and effective design of patient care. Providing a work environment that is safe and free of ergonomic stressors, allowing staff to interact with technology and devices in a way that enhances and does not complicate their work, is the primary goal of clinically informed human factors engineering.
As part of a total systems approach to safety, understanding the impact of inequities on vulnerable populations is the responsibility of all healthcare organization leaders. Leaders must take a data-driven approach to learn where gaps and opportunities to improve health equity exist. Advancing healthcare equity, identified as the fifth element in the Quintuple Aim, has become even more critical since the pandemic exposed how socially marginalized populations experience higher COVID-19 morbidity and mortality.
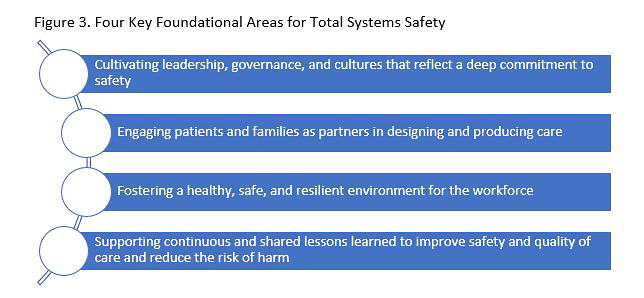
Implementing a total systems approach to safety is challenging and requires strategic planning and objectives. As a member of the National Steering Committee for Patient Safety, ECRI helped design the National Action Plan to Advance Patient Safety. The Action Plan lays out a strategy for organizations to implement four key areas that create the foundation that total systems safety can be built on. Described in Figure 3, the four foundational areas are:
- Leadership, culture, and governance
- Patient and family engagement
- Workforce safety
- Learning system
Total Systems Approach to Reducing Harm Related to Staffing Shortages
ECRI recommends that healthcare leaders organize and focus key efforts to mitigate the impact of the healthcare staffing shortage on patient and workforce safety. In a total systems approach to safety, leadership should be aligned with and fully supportive of the system redesign needed to improve the culture of safety and achieve safety goals. Before embarking on improvement efforts, it is imperative that organizations have both leadership commitment and staff engagement to drive the changes needed to address factors that lead to staffing shortages.
Based on the four foundational areas, ECRI recommends that healthcare organizations do the following:
Leadership, Culture, and Governance
Recommendations:
- Develop organizational staffing safety goals that have a dedicated executive sponsor and are accompanied by a detailed action plan and metrics (e.g., staffing vacancy rates)
- Build a diverse, inclusive, culturally competent workforce that promotes health equity
- Evaluate the effect of staffing ratios on incidents and outcomes
- Develop career progression pathways to promote the growth of clinical leaders within the organization
Patient and Family Engagement
Recommendations:
- Develop flexible action plans to deliver safe patient care during staffing shortages, including closing units or diverting patients
- Use patient advocates to help support creative models that help staff understand the needs and concerns of patients and families
- Utilize patient and family advisory councils to solicit feedback regarding how care is provided in times of staffing shortages while examining trends to identify areas of opportunity
Workforce Safety
Recommendations:
- Establish flexible staffing models to reduce the dependency on temporary staffing
- Design the system to respond to staff needs and assess for psychological safety
- Invest in technology to minimize staffing burden associated with tracking and managing recalls and safety hazards
- Use human-factors engineering to standardize efficient workflows for safer use, care, and cleaning of medical supplies and equipment
Learning System
Recommendations:
- Evaluate near misses and safety events to identify risks and contributing factors associated with staffing shortages
- Conduct surveys to better understand staff perspectives on staffing shortages
- Design flexible onboarding and training programs for both permanent and temporary staff
- Implement daily huddles to review safety concerns and hassles. Include traveler/agency and float staff in the huddles
A Final Word
In summary, a total systems approach to safety is one that leverages the principles of system design, human-factors engineering, health equity, and advanced safety science. When applied to the four foundational areas of leadership, culture, and governance; patient and family engagement; workforce safety; and learning systems, it is a powerful model to drive improvement of high complexity problems, including staffing shortages.